In vitro fertilization
What is IVF?
In vitro fertilization (IVF) is a reproductive technology in which conception, early embryo development, and formation occur in laboratory conditions outside the mother’s body. This method is sought after when a woman or a man is experiencing infertility or severe pathologies that prevent them from conceiving a child naturally. The procedure carries certain risks, so IVF should only be performed in accredited clinics following the appropriate protocol.
Before the procedure, both spouses must undergo examinations. Women are recommended to undergo a complete blood analysis, hormone testing, coagulogram, screenings for urogenital infections (mycoplasmosis, ureaplasmosis, chlamydia, trichomoniasis), as well as ultrasound and colposcopy. Men are required to provide a semen analysis. It is important for both spouses to consult a geneticist and undergo tests for HIV, syphilis, and hepatitis C.
How is the procedure performed?

Ovarian Stimulation
It is based on the medical suppression of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) secretion. This stimulates the ovaries to produce multiple follicles containing eggs.

Oocyte Retrieval
Follicles are punctured, and the eggs are collected and placed in a nutrient-rich medium. They are then placed in an incubator with conditions similar to the woman’s uterus.
Preparation of Gametes
The maturity and structure of the eggs are assessed, and spermatozoa are processed and selected for fertilization.

Fertilization of Eggs
There are two methods of fertilizing the eggs.
Conventional IVF. The male and female gametes are placed in a specialized thermostat filled with an embryo culture medium (containing approximately 40 different substances). Here, the sperm penetrates the egg, leading to fertilization.
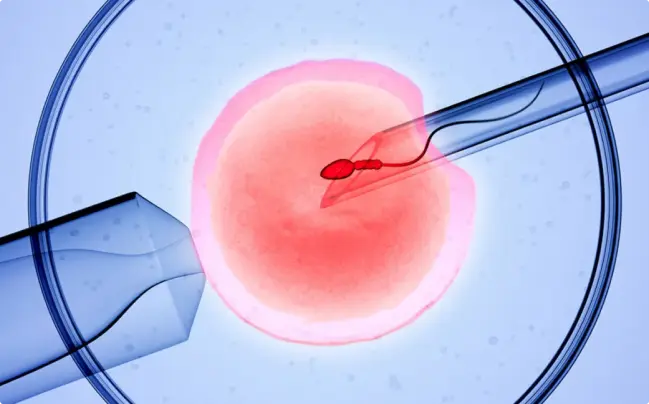
Intracytoplasmic Sperm Injection (ICSI). A healthy and active sperm is injected into the egg using a fine needle.

Embryo Transfer to the Uterine Cavity
Embryo transfer typically occurs on day 2-3 or day 5-6 of the cultivation process. Under ultrasound guidance, the embryos are transferred into the uterus using a thin catheter.

Luteal Phase Support
To support the luteal phase, the woman receives progesterone hormone supplementation.
Who requires the IVF procedure?
Indications for IVF include infertility with the absence of pregnancy for 1.5-2 years in women who are sexually active without the use of contraceptives. There are several forms of infertility, including:
Immunological
Factors related to the woman’s immune system affect the male gametes.
Hormonal
Inability to conceive due to an endocrine system malfunction.
Idiopathic
Failure to achieve pregnancy despite no detectable health issues in the woman.
In addition, IVF is indicated in the following cases:
Endometriosis
Pathological growth of the endometrium that can affect surrounding organs such as the ovaries, fallopian tubes, rectum, or bladder. It can cause ovulation disorders and pathological changes in the fallopian tubes and ovaries, leading to a reduced chance of pregnancy.
Pituitary tumors
Tumors in the pituitary gland, a major endocrine organ responsible for reproductive function, can cause conditions such as amenorrhea (absence of menstruation), shortened menstrual cycles (3 days or less), and intermenstrual bleeding in women.
Congenital defects of the reproductive organs
These include bicornuate or septate uterus, absence or occlusion of the vagina, and complete or partial uterine septum, which can hinder or make pregnancy and fetal development impossible.
Genital tuberculosis
Bacterial infection primarily affecting the fallopian tubes and endometrium, less commonly the ovaries, cervix, or vagina. Infertility is a common symptom of genital tuberculosis, along with menstrual cycle disorders such as oligomenorrhea (infrequent periods), amenorrhea (absence of menstruation for more than 6 months), and dysmenorrhea (painful periods).
Systemic autoimmune diseases
Conditions like type 1 diabetes, systemic lupus erythematosus, vasculitis, rheumatoid arthritis, and Crohn’s disease can indirectly affect fertility and require IVF.
IVF can also be recommended for male infertility or conditions such as:
- Obstructive infertility: Issues related to the passage of sperm through the male reproductive system.
- Ejaculatory disorders: Conditions like retrograde ejaculation, where semen is not ejaculated through the penis but goes into the bladder.
- Azoospermia: Absence of sperm in the ejaculate.
- High risk of genetic diseases transmission.
Psychosocial disorders can also indirectly impact fertility. These include persistent or periodic fear of sexual intimacy, resulting in frequent refusal of sexual activity; orgasmic disorders; pain during sexual intercourse; and vaginismus, an involuntary spasm of the vaginal muscles during penetration. Hormonal imbalances, prolonged stress, depression, and inflammation in the pelvic organs can contribute to these conditions.
When is IVF contraindicated?
In certain cases, IVF is not recommended if a woman has the following pathological conditions:
- Absence or malformation of the uterus;
- Individual intolerance to medications used in the artificial fertilization program;
- Other diseases affecting organs and systems that may pose a risk of miscarriage or threaten the woman’s life:
- such as cardiovascular diseases (heart defects, hypertension);
- disorders of the circulatory or endocrine system;
- kidney or liver pathologies, or any form of cancer.
- Mental disorders.
For men, contraindications include:
- Genetic diseases with a high risk of transmission to offspring;
- Low sperm viability or absence of sperm in the ejaculate;
- Presence of cancer or upcoming chemotherapy or radiation therapy.
However, some of these issues can be addressed through modern technologies and methods. For example, to prevent the risk of transmitting a genetic disease, preimplantation genetic diagnosis (PGD) is performed before IVF to identify embryos with abnormalities.
Risks and Side Effects of IVF
Like any medical intervention, IVF carries certain risks, including:
Ectopic or multiple pregnancies
Ectopic pregnancy occurs when the fertilized egg implants outside the uterus, in the abdominal cavity, ovary, fallopian tube, or cervix. The danger lies in the rupture of the organ where the egg has attached, leading to severe bleeding that can be life-threatening. In the case of multiple pregnancies, the risks increase:
- Miscarriage.
- Death of one of the embryos, which can result in the cessation of development of the other embryo.
- Preterm labor, which can lead to complications associated with prematurity.
Ovarian hyperstimulation syndrome
This condition involves a significant enlargement of the ovaries, which can lead to their rupture. There is also a risk of thrombosis, kidney failure, and fluid accumulation in the abdomen, requiring immediate hospitalization.
Abnormal fetal development
Despite the reduced risk with PGD, there is still a possibility of giving birth to children with developmental abnormalities such as brain ischemia, Down syndrome, or other congenital defects.
To ensure a successful IVF procedure for prospective parents, it is crucial to choose a reputable clinic with experienced specialists. It is important that doctors carefully consider the woman’s health and perform the procedure taking into account her individual characteristics.